

SUBSCRIBE TO OUR FREE NEWSLETTER
Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.
5
#000000
#FFFFFF
To donate by check, phone, or other method, see our More Ways to Give page.


Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.

A woman enters La Colaborativa vaccine clinic in Chelsea, Massachusetts on February 16, 2021. (Photo: Joseph Prezioso/AFP via Getty Images)
During the first 2.5 months of coronavirus vaccine distribution within the U.S., counties with higher levels of poverty and other indicators of socioeconomic vulnerability were inoculated at lower rates, a new analysis shows.
The report, published Wednesday by the Centers for Disease Control and Prevention (CDC), compares county-level estimates of first-dose vaccination coverage--the percentage of people in a county who had received at least one dose of a Covid-19 vaccine between mid-December and early March--with county-level measures of social vulnerability.
"Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
--CDC
According to the study, "Covid-19 vaccination coverage was lower in high-vulnerability counties than in low-vulnerability counties, a finding largely driven by socioeconomic disparities."
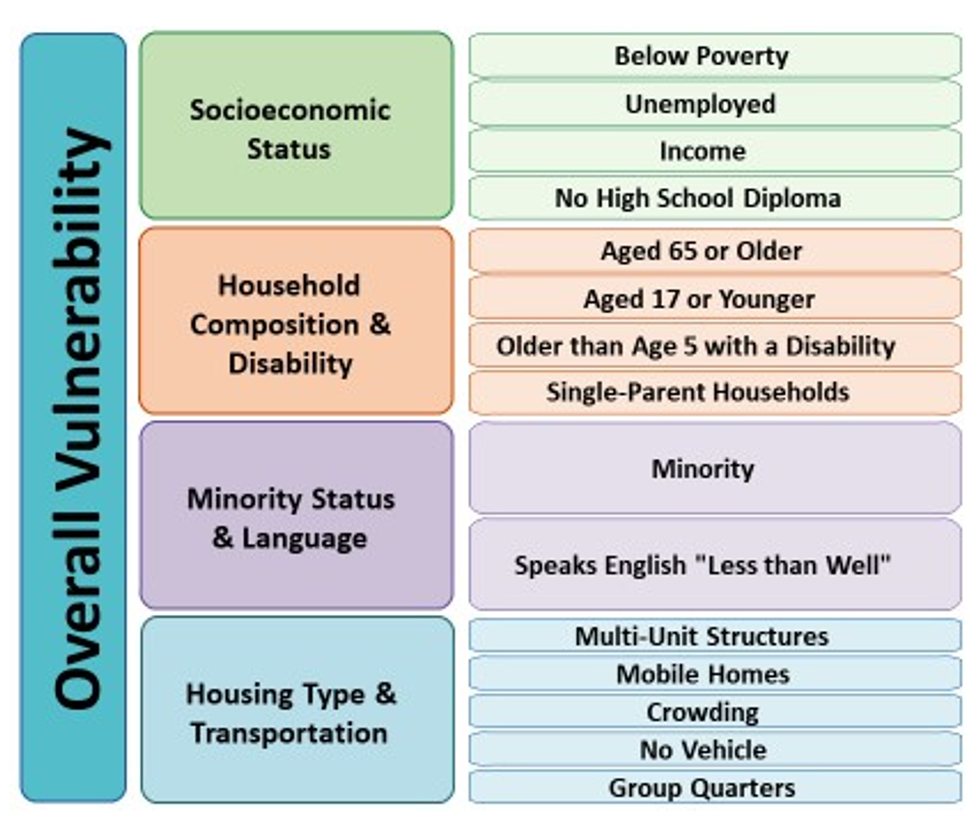
Comprised of 15 metrics that are categorized into four themes, the CDC's Social Vulnerability Index (SVI) combines census data on key socioeconomic and demographic variables--including income; educational attainment; household composition in terms of age and disability; prevalence of marginalized racial and linguistic groups; and housing and transportation characteristics--in an effort to minimize suffering during disasters by improving communities' preparation for and responses to hazardous events, including epidemics.
Last year, the National Academies of Sciences, Engineering, and Medicine recommended that the Department of Health and Human Services and state, tribal, local, and territorial governments use the SVI as a tool to ensure the equitable allocation of Covid-19 vaccines.
Nationally, a total of 51,873,700 residents of 49 states and D.C. received at least one dose of a Covid-19 vaccine between December 14 and March 1--a coverage rate of 15.1%. The study found that vaccination coverage was higher in low-vulnerability counties than in high-vulnerability counties, although a few states had more equitable coverage, and patterns varied further when indicators were disaggregated.
For the overall SVI measure, there was a vaccination coverage gap of 1.9 percentage points between low-vulnerability counties (15.8%) and high-vulnerability counties (13.9%).
While the general pattern of unequal inoculation rates was found across three of the four SVI themes, some factors were associated with greater disparities.
The most pronounced vaccine inequities, for instance, corresponded with socioeconomic status, which yielded a gap of 2.5 percentage points between low-vulnerability counties and high-vulnerability counties. Among socioeconomic status indicators, the most impactful variable was the percentage of adults without a high school diploma, which was associated with a difference of 2.8 percentage points between low- and high-vulnerability counties.
Meanwhile, for three indicators--population aged 65 and older, multi-unit housing, and households without a vehicle--vaccination coverage was slightly higher in high-vulnerability counties.
While "higher coverage in counties with large proportions of older adults was consistent with the prioritization of this age group early in the vaccination program," the researchers wrote, "the higher coverage in counties with lower percentages of households with a vehicle available was unexpected and warrants further investigation."
With respect to two indicators--percentages of people with disabilities and individuals who speak English "less than well"--inoculation rates were roughly the same in low- and high-vulnerability counties, a finding the researchers described as "encouraging in light of the disproportionate incidence of Covid-19 in these populations."
Regarding the remaining 10 indicators, however, vaccination coverage was higher in low-vulnerability counties, demonstrating that "equity in access to Covid-19 vaccination has not been achieved nationwide," as the report's authors put it.
For the overall SVI measure, vaccine inequities were found in 31 states, including 11 where disparities were identified in all four themes.
"Additional efforts are needed to achieve equity in vaccination coverage for those who have been most affected by Covid-19," wrote the authors of the report.
"Improving Covid-19 vaccination coverage in communities with high proportions of racial/ethnic minority groups and persons who are economically and socially marginalized is critical," they added, "because these populations have been disproportionately affected by Covid-19-related morbidity and mortality."
According to the researchers, "Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
"Public health officials can investigate whether disparities are occurring because of access problems (e.g., vaccine supply, vaccination clinic availability, and lack of prioritization of vulnerable groups) or other challenges, such as vaccine hesitancy," they wrote. "Vaccination promotion, outreach, and administration might focus on high-vulnerability populations within counties (e.g., providing resources to federally qualified health centers when socioeconomic disparities are identified)."
Arizona and Montana were the only two states to equitably distribute vaccines by allocating doses at higher rates in high-vulnerability counties across all aspects of the SVI.
Three additional states had higher vaccination coverage in high-vulnerability counties than in low-vulnerability counties for the overall SVI measure and in three of four themes. Alaska fell short in the socioeconomic status theme, while Minnesota and West Virginia had shortcomings in the racial minority and language theme.
According to the report, practices in states with more equitable vaccination coverage included:
After acknowledging the study's limitations--including state-level variations in prioritization policies, a lack of individual-level vulnerability data, and the existence of intra-county inequalities, among others--the authors concluded with a recommendation.
"As vaccine supply increases and administration expands to additional priority groups," the researchers wrote, "CDC, state, and local jurisdictions should continue to monitor vaccination levels by SVI metrics to aid in the development of community efforts to improve vaccination access, outreach, and administration among populations most affected by Covid-19."
Dear Common Dreams reader, The U.S. is on a fast track to authoritarianism like nothing I've ever seen. Meanwhile, corporate news outlets are utterly capitulating to Trump, twisting their coverage to avoid drawing his ire while lining up to stuff cash in his pockets. That's why I believe that Common Dreams is doing the best and most consequential reporting that we've ever done. Our small but mighty team is a progressive reporting powerhouse, covering the news every day that the corporate media never will. Our mission has always been simple: To inform. To inspire. And to ignite change for the common good. Now here's the key piece that I want all our readers to understand: None of this would be possible without your financial support. That's not just some fundraising cliche. It's the absolute and literal truth. We don't accept corporate advertising and never will. We don't have a paywall because we don't think people should be blocked from critical news based on their ability to pay. Everything we do is funded by the donations of readers like you. Will you donate now to help power the nonprofit, independent reporting of Common Dreams? Thank you for being a vital member of our community. Together, we can keep independent journalism alive when it’s needed most. - Craig Brown, Co-founder |
During the first 2.5 months of coronavirus vaccine distribution within the U.S., counties with higher levels of poverty and other indicators of socioeconomic vulnerability were inoculated at lower rates, a new analysis shows.
The report, published Wednesday by the Centers for Disease Control and Prevention (CDC), compares county-level estimates of first-dose vaccination coverage--the percentage of people in a county who had received at least one dose of a Covid-19 vaccine between mid-December and early March--with county-level measures of social vulnerability.
"Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
--CDC
According to the study, "Covid-19 vaccination coverage was lower in high-vulnerability counties than in low-vulnerability counties, a finding largely driven by socioeconomic disparities."
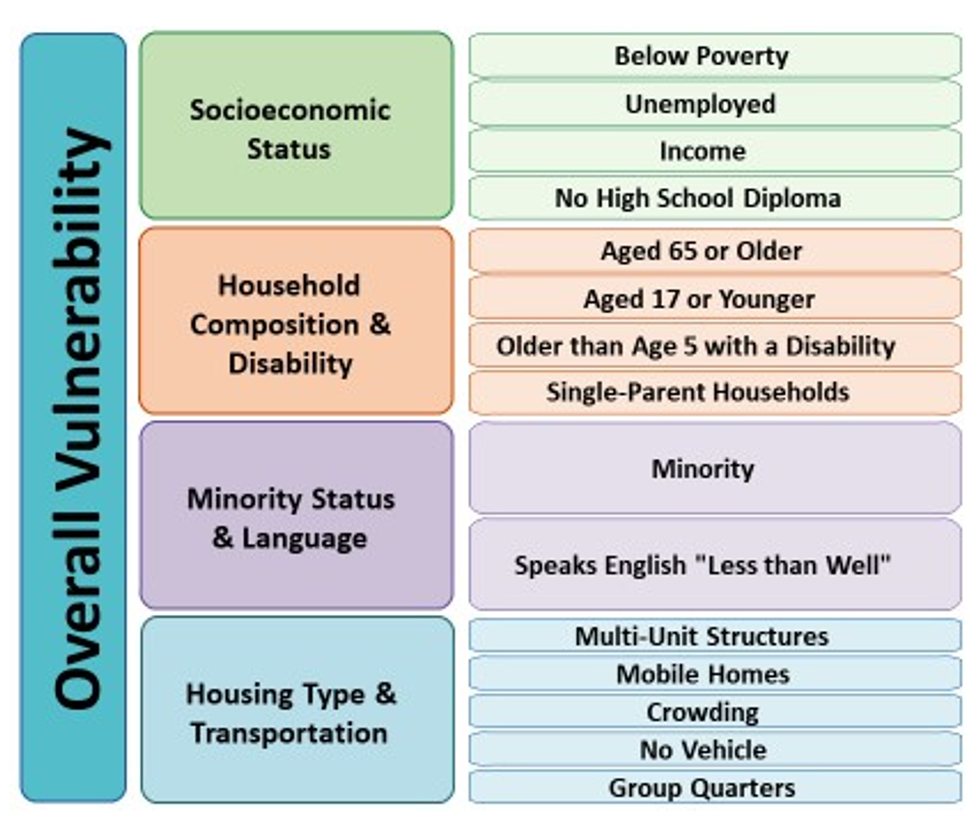
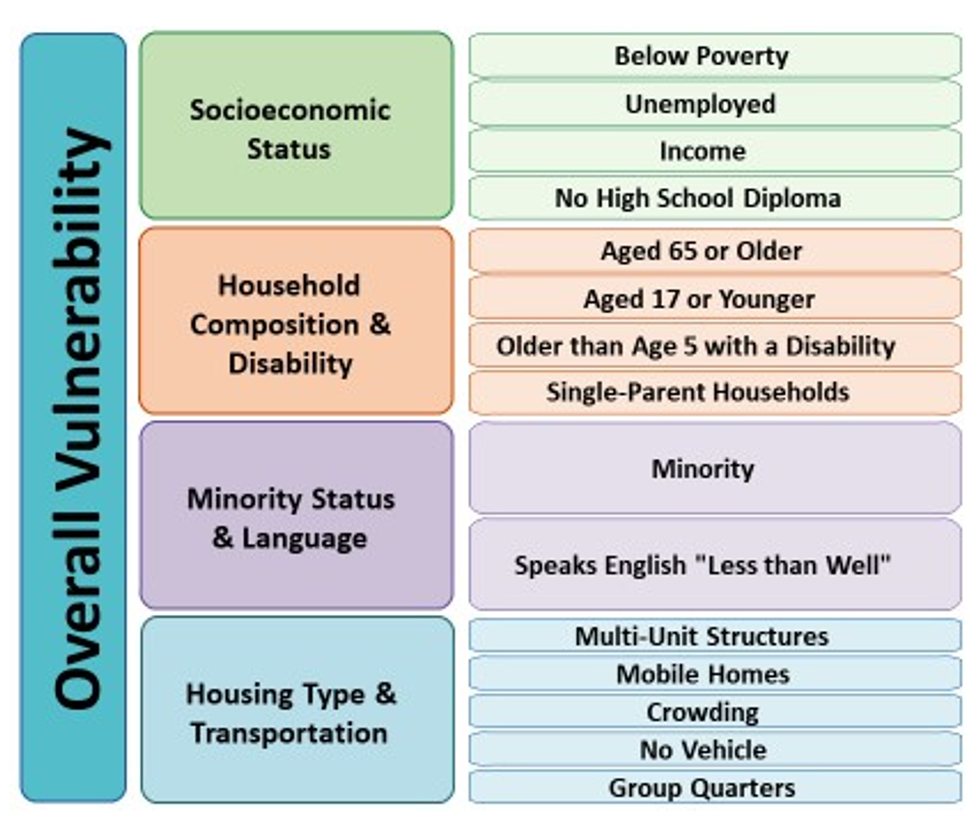
Comprised of 15 metrics that are categorized into four themes, the CDC's Social Vulnerability Index (SVI) combines census data on key socioeconomic and demographic variables--including income; educational attainment; household composition in terms of age and disability; prevalence of marginalized racial and linguistic groups; and housing and transportation characteristics--in an effort to minimize suffering during disasters by improving communities' preparation for and responses to hazardous events, including epidemics.
Last year, the National Academies of Sciences, Engineering, and Medicine recommended that the Department of Health and Human Services and state, tribal, local, and territorial governments use the SVI as a tool to ensure the equitable allocation of Covid-19 vaccines.
Nationally, a total of 51,873,700 residents of 49 states and D.C. received at least one dose of a Covid-19 vaccine between December 14 and March 1--a coverage rate of 15.1%. The study found that vaccination coverage was higher in low-vulnerability counties than in high-vulnerability counties, although a few states had more equitable coverage, and patterns varied further when indicators were disaggregated.
For the overall SVI measure, there was a vaccination coverage gap of 1.9 percentage points between low-vulnerability counties (15.8%) and high-vulnerability counties (13.9%).
While the general pattern of unequal inoculation rates was found across three of the four SVI themes, some factors were associated with greater disparities.
The most pronounced vaccine inequities, for instance, corresponded with socioeconomic status, which yielded a gap of 2.5 percentage points between low-vulnerability counties and high-vulnerability counties. Among socioeconomic status indicators, the most impactful variable was the percentage of adults without a high school diploma, which was associated with a difference of 2.8 percentage points between low- and high-vulnerability counties.
Meanwhile, for three indicators--population aged 65 and older, multi-unit housing, and households without a vehicle--vaccination coverage was slightly higher in high-vulnerability counties.
While "higher coverage in counties with large proportions of older adults was consistent with the prioritization of this age group early in the vaccination program," the researchers wrote, "the higher coverage in counties with lower percentages of households with a vehicle available was unexpected and warrants further investigation."
With respect to two indicators--percentages of people with disabilities and individuals who speak English "less than well"--inoculation rates were roughly the same in low- and high-vulnerability counties, a finding the researchers described as "encouraging in light of the disproportionate incidence of Covid-19 in these populations."
Regarding the remaining 10 indicators, however, vaccination coverage was higher in low-vulnerability counties, demonstrating that "equity in access to Covid-19 vaccination has not been achieved nationwide," as the report's authors put it.
For the overall SVI measure, vaccine inequities were found in 31 states, including 11 where disparities were identified in all four themes.
"Additional efforts are needed to achieve equity in vaccination coverage for those who have been most affected by Covid-19," wrote the authors of the report.
"Improving Covid-19 vaccination coverage in communities with high proportions of racial/ethnic minority groups and persons who are economically and socially marginalized is critical," they added, "because these populations have been disproportionately affected by Covid-19-related morbidity and mortality."
According to the researchers, "Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
"Public health officials can investigate whether disparities are occurring because of access problems (e.g., vaccine supply, vaccination clinic availability, and lack of prioritization of vulnerable groups) or other challenges, such as vaccine hesitancy," they wrote. "Vaccination promotion, outreach, and administration might focus on high-vulnerability populations within counties (e.g., providing resources to federally qualified health centers when socioeconomic disparities are identified)."
Arizona and Montana were the only two states to equitably distribute vaccines by allocating doses at higher rates in high-vulnerability counties across all aspects of the SVI.
Three additional states had higher vaccination coverage in high-vulnerability counties than in low-vulnerability counties for the overall SVI measure and in three of four themes. Alaska fell short in the socioeconomic status theme, while Minnesota and West Virginia had shortcomings in the racial minority and language theme.
According to the report, practices in states with more equitable vaccination coverage included:
After acknowledging the study's limitations--including state-level variations in prioritization policies, a lack of individual-level vulnerability data, and the existence of intra-county inequalities, among others--the authors concluded with a recommendation.
"As vaccine supply increases and administration expands to additional priority groups," the researchers wrote, "CDC, state, and local jurisdictions should continue to monitor vaccination levels by SVI metrics to aid in the development of community efforts to improve vaccination access, outreach, and administration among populations most affected by Covid-19."
During the first 2.5 months of coronavirus vaccine distribution within the U.S., counties with higher levels of poverty and other indicators of socioeconomic vulnerability were inoculated at lower rates, a new analysis shows.
The report, published Wednesday by the Centers for Disease Control and Prevention (CDC), compares county-level estimates of first-dose vaccination coverage--the percentage of people in a county who had received at least one dose of a Covid-19 vaccine between mid-December and early March--with county-level measures of social vulnerability.
"Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
--CDC
According to the study, "Covid-19 vaccination coverage was lower in high-vulnerability counties than in low-vulnerability counties, a finding largely driven by socioeconomic disparities."
Comprised of 15 metrics that are categorized into four themes, the CDC's Social Vulnerability Index (SVI) combines census data on key socioeconomic and demographic variables--including income; educational attainment; household composition in terms of age and disability; prevalence of marginalized racial and linguistic groups; and housing and transportation characteristics--in an effort to minimize suffering during disasters by improving communities' preparation for and responses to hazardous events, including epidemics.
Last year, the National Academies of Sciences, Engineering, and Medicine recommended that the Department of Health and Human Services and state, tribal, local, and territorial governments use the SVI as a tool to ensure the equitable allocation of Covid-19 vaccines.
Nationally, a total of 51,873,700 residents of 49 states and D.C. received at least one dose of a Covid-19 vaccine between December 14 and March 1--a coverage rate of 15.1%. The study found that vaccination coverage was higher in low-vulnerability counties than in high-vulnerability counties, although a few states had more equitable coverage, and patterns varied further when indicators were disaggregated.
For the overall SVI measure, there was a vaccination coverage gap of 1.9 percentage points between low-vulnerability counties (15.8%) and high-vulnerability counties (13.9%).
While the general pattern of unequal inoculation rates was found across three of the four SVI themes, some factors were associated with greater disparities.
The most pronounced vaccine inequities, for instance, corresponded with socioeconomic status, which yielded a gap of 2.5 percentage points between low-vulnerability counties and high-vulnerability counties. Among socioeconomic status indicators, the most impactful variable was the percentage of adults without a high school diploma, which was associated with a difference of 2.8 percentage points between low- and high-vulnerability counties.
Meanwhile, for three indicators--population aged 65 and older, multi-unit housing, and households without a vehicle--vaccination coverage was slightly higher in high-vulnerability counties.
While "higher coverage in counties with large proportions of older adults was consistent with the prioritization of this age group early in the vaccination program," the researchers wrote, "the higher coverage in counties with lower percentages of households with a vehicle available was unexpected and warrants further investigation."
With respect to two indicators--percentages of people with disabilities and individuals who speak English "less than well"--inoculation rates were roughly the same in low- and high-vulnerability counties, a finding the researchers described as "encouraging in light of the disproportionate incidence of Covid-19 in these populations."
Regarding the remaining 10 indicators, however, vaccination coverage was higher in low-vulnerability counties, demonstrating that "equity in access to Covid-19 vaccination has not been achieved nationwide," as the report's authors put it.
For the overall SVI measure, vaccine inequities were found in 31 states, including 11 where disparities were identified in all four themes.
"Additional efforts are needed to achieve equity in vaccination coverage for those who have been most affected by Covid-19," wrote the authors of the report.
"Improving Covid-19 vaccination coverage in communities with high proportions of racial/ethnic minority groups and persons who are economically and socially marginalized is critical," they added, "because these populations have been disproportionately affected by Covid-19-related morbidity and mortality."
According to the researchers, "Monitoring community-level metrics is essential to informing tailored, local vaccine delivery efforts, which might reduce inequities."
"Public health officials can investigate whether disparities are occurring because of access problems (e.g., vaccine supply, vaccination clinic availability, and lack of prioritization of vulnerable groups) or other challenges, such as vaccine hesitancy," they wrote. "Vaccination promotion, outreach, and administration might focus on high-vulnerability populations within counties (e.g., providing resources to federally qualified health centers when socioeconomic disparities are identified)."
Arizona and Montana were the only two states to equitably distribute vaccines by allocating doses at higher rates in high-vulnerability counties across all aspects of the SVI.
Three additional states had higher vaccination coverage in high-vulnerability counties than in low-vulnerability counties for the overall SVI measure and in three of four themes. Alaska fell short in the socioeconomic status theme, while Minnesota and West Virginia had shortcomings in the racial minority and language theme.
According to the report, practices in states with more equitable vaccination coverage included:
After acknowledging the study's limitations--including state-level variations in prioritization policies, a lack of individual-level vulnerability data, and the existence of intra-county inequalities, among others--the authors concluded with a recommendation.
"As vaccine supply increases and administration expands to additional priority groups," the researchers wrote, "CDC, state, and local jurisdictions should continue to monitor vaccination levels by SVI metrics to aid in the development of community efforts to improve vaccination access, outreach, and administration among populations most affected by Covid-19."