

SUBSCRIBE TO OUR FREE NEWSLETTER
Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.
5
#000000
#FFFFFF
To donate by check, phone, or other method, see our More Ways to Give page.


Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.
"Republicans in Congress and President Trump are focused on spending $1 billion a day on a needless war with Iran that is already jacking up prices for Americans," noted one expert.
President Donald Trump made clear in a new interview with Politico that he either doesn't understand or won't accept the US public's response to his and Israel's war on Iran, which they're waging while Americans face rising unemployment and gasoline prices on top of high costs for other essentials, from groceries to housing.
According to Politico White House bureau chief Dasha Burns:
Speaking in a phone call Thursday, Trump was entirely on offense. He brushed off worries about the impact of the Iran war on gas prices and US ammunition reserves, and he insisted that the military onslaught was popular with voters. Many recent public polls show the opposite is true, although a survey released Thursday by Fox News found voters have mixed opinions on Iran...
"People are loving what's happening," Trump said. "We're taking out a threat to the United States of America, major threat... and doing it like nobody's ever seen before."
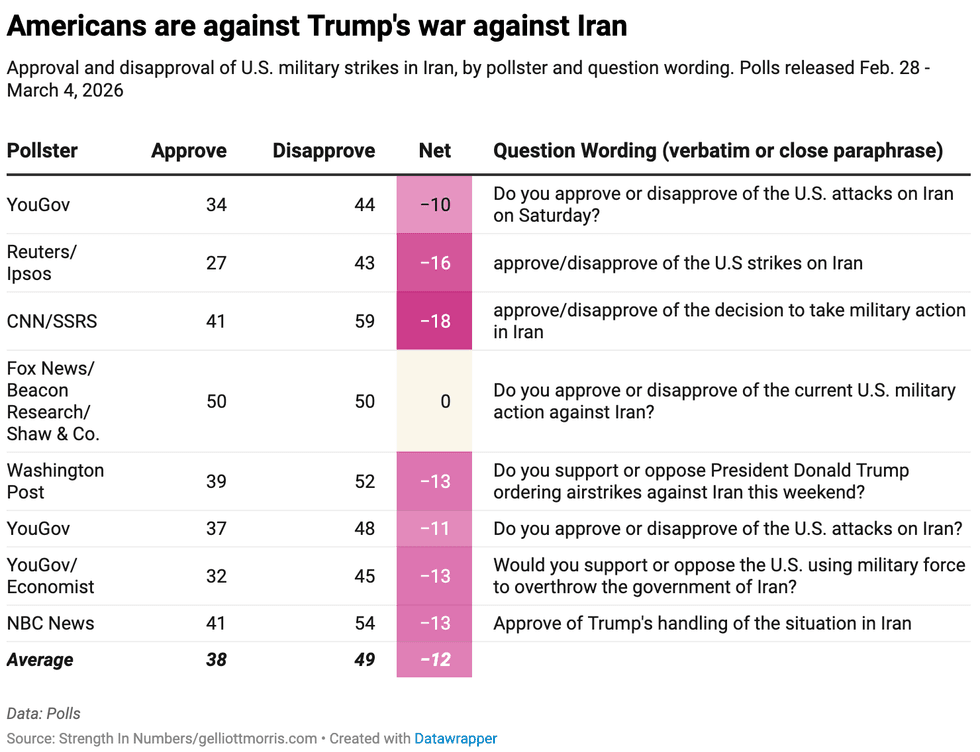
A roundup of recent polling collected and published Friday by Strength in Numbers data journalist G. Elliott Morris shows roughly half of Americans disapprove of the war on Iran, while only 38% approve.
Despite the polling, the GOP-controlled Congress has refused to rein in Trump's assault on Iran. Democratic US Sen. John Fetterman (Pa.) and four Democrats in the House of Representatives—Congressmen Henry Cuellar (Texas), Jared Golden (Maine), Greg Landsman (Ohio), and Juan Vargas (Calif.)—voted with nearly all Republicans this week to block a pair of war powers resolutions.
In the interview with Politico, Trump described the Iranian military as "decimated," and said that "we'll work with the people and the regime to make sure that somebody gets there that can nicely build Iran but without nuclear weapons."
As of Thursday, the Iranian government put the death toll at 1,230 people, including around 175 killed in a reported "double-tap" strike on a girls' elementary school. Israel has denied responsibility and top US officials have only said they're looking into it. A New York Times analysis concluded that the United States was "most likely to have carried out the strike," which killed mostly children. According to Reuters, US investigators also believe that American forces were behind the bombing.
Separately, the Times reported that two boys' schools—one elementary and one middle—southwest of Tehran "appeared to have been damaged on Thursday during the bombing campaign being conducted by the United States and Israel," though unlike with the earlier attack in Minab, "there were no immediate reports of deaths or injuries."
In addition to discussing Iran, Trump told Politico that "Cuba's going to fall, too," but "they want to make a deal." He also addressed Venezuela, whose president was recently abducted by US forces and replaced with a deputy who agreed to let Trump control the nationalized oil industry; his frustration with Ukrainian President Volodymyr Zelenskyy, who continues to combat a Russian invasion; and his recent spat with the artificial intelligence company Anthropic, which the president "fired" because of its refusal to let the Pentagon end the AI firm's policies against autonomous killer robots and mass surveillance of Americans.
With Trump focused on various conflicts abroad, Americans are contending with some of the consequences, including the impact on petroleum. Business Insider reported Friday that "the national average price for a gallon of regular gasoline climbed to $3.32 on Friday, according to AAA—that's an 11.4% increase from last week's price and the highest level since August 2024."
Meanwhile, the US Bureau of Labor Statistics revealed Friday that the US economy lost 92,000 jobs last month.
"Trump's reckless economic agenda has forced the labor market into the negative, threatening the livelihoods of American workers," responded Alex Jacquez, a former Obama administration official who's now chief of policy and advocacy at Groundwork Collaborative. "As the president piles on blanket tariffs and oil prices soar, today's report confirms he's sent the economy straight into a stagflation spiral."
The new jobs data came after the Wall Street Journal reported Wednesday that a record number of US workers are raiding their retirement savings. The top reasons for the surge in 401(k) withdrawals were avoiding eviction or paying off medical expenses.
Americans are facing an even more dire healthcare situation this year, due to Medicaid cuts in Trump and congressional Republicans' so-called One Big Beautiful Bill Act—which also gave the rich more tax breaks—as well as their refusal to extend expired Affordable Care Act subsidies that helped tens of millions of people pay for health insurance.
"We should all be concerned about the slowing economy we've seen in the second Trump administration," Angela Hanks, a former Department of Labor official who's now chief of policy programs at the Century Foundation, said Friday. "The economy lost thousands of jobs this month including in healthcare and social services, the main sectors previously propping up the labor market."
"Healthcare, childcare, and manufacturing—sectors Americans rely on—all lost jobs last month with no plan from the Trump administration on how to fix it," Hanks added. "Meanwhile, Republicans in Congress and President Trump are focused on spending $1 billion a day on a needless war with Iran that is already jacking up prices for Americans."
"We don't allow banks to call themselves the U.S. Treasury Investment Fund," said Rep. Mark Pocan. "We don't allow anyone to call themselves USPS Plus. So why allow insurance companies to call private insurance Medicare Advantage?"
A group of Democratic lawmakers on Wednesday reintroduced legislation aimed at reining in for-profit insurance companies who use the Medicare name to market their plans.
The "Save Medicare Act," being reintroduced by US Reps. Mark Pocan (D-Wis.), Ro Khanna (D-Calif.), and Jan Schakowsky (D-Ill.), bars private insurers from using the word "Medicare" in marketing their plans, imposing "significant fines" for any insurer that doesn't comply.
At issue, the lawmakers said, is that insurers are flooding the airwaves with ads for Medicare Advantage plans during open enrollment periods. The ads are deceiving Americans into thinking their plans are just variations of Medicare services offered by the federal government, they said.
"Let’s be clear: Medicare Advantage is not Medicare," said Schakowsky. "These private insurance plans use Medicare’s trusted name while too often denying medically necessary care, restricting providers, and overcharging taxpayers by billions. That is unacceptable. We have seen insurers exploit the system to boost profits at the expense of seniors."
Khanna noted that Medicare Advantage is "a private insurance program that too often boosts profits by limiting coverage," even as it "misleads seniors into thinking it's traditional Medicare."
"That's wrong," Khanna emphasized. "This legislation will stop private insurers from cashing in on the Medicare name. We should be working to protect and expand real Medicare instead."
Pocan declared that "only Medicare is Medicare," adding that Medicare Advantage plans "often leave patients without the benefits they need while overcharging the federal government for corporate profit."
"This bill makes clear what is—and what is not—Medicare," added Pocan, "and ensures this essential program will continue to serve seniors and other Americans for generations to come."
Pocan also posted a video on social media where he talked about his elderly mother being unable to see the physician that came to her assisted living home because she relied on Medicare Advantage and the doctor in question was out of network.
"She would have had to go all the way across town to get that care," Pocan explained. "The problem is, she wasn't very mobile and she never got the medical care."
We don't allow banks to call themselves the U.S. Treasury Investment Fund. We don't allow anyone to call themselves USPS Plus.
So why allow insurance companies to call private insurance Medicare Advantage?
I’m reintroducing the Save Medicare Act with @RepRoKhanna and… pic.twitter.com/c6dAXpEJqY
— Rep. Mark Pocan (@RepMarkPocan) March 4, 2026
"We don't allow banks to call themselves the U.S. Treasury Investment Fund," said Pocan. "We don't allow anyone to call themselves USPS Plus. So why allow insurance companies to call private insurance Medicare Advantage?"
Many progressive critics have for years pointed to Medicare Advantage as a legitimate example of wasteful spending by the federal government.
A report released in January by the Medicare Payment Advisory Commission (MedPAC), an independent congressional agency that advises lawmakers on Medicare, estimated that overpayments to Medicare Advantage plans could total $76 billion in 2026.
One major factor in the overpayments is that patients using Medicare Advantage plans tend to be healthier than patients on traditional Medicare, with the result being that private insurers charge the government more than is necessary to meet these patients' needs.
On Wednesday, Schakowsky said that the "crucial legislation" she joined Khanna and Pocan in introducing "will end deceptive marketing and ensure beneficiaries understand the difference between traditional Medicare and private insurance plans."
"Seniors deserve transparency, accountability, and the full benefits they have earned," she said.
We often talk about immigrants as beneficiaries of American opportunity. But in higher education, healthcare, research and beyond, immigrants are also architects of institutional improvement.
The US Department of Education recently withdrew its unlawful directive that would have restricted diversity, equity, and inclusion efforts in schools and universities nationwide. The guidance was framed as an attempt to enforce “neutrality” in education. In practice, it would have narrowed how institutions identify and address inequity, discouraging efforts to create learning environments that reflect the realities of an increasingly global student population.
That national debate can feel abstract, just another skirmish in a broader culture war over higher education. But equity is not abstract. It lives in the quiet mechanics of institutions: who gets seen, who gets filtered out, and which barriers are treated as incidental rather than structural. I am reminded of this not by a court ruling or federal directive, but in the ordinary work of teaching and mentoring students from around the world as an assistant professor at the University of Illinois Urbana-Champaign. It shows up during office hours, committee meetings, and the quiet moments when institutional rules do their work.
Americans are fluent in a familiar story about immigration: Immigrants come to the United States for opportunity—better education, better jobs, better lives. That story is not wrong. But it is incomplete. What is talked about far less is how immigrants improve the institutions they enter, often by exposing the limits of systems that were never designed with them in mind.
Case in point: Like many graduate programs, ours used procedures that filtered out applicants who had not paid an application fee before faculty review. When they failed to pay, I was never supposed to see their application. The fee, common by US standards, was prohibitively expensive in some local currencies. Until I learned about that procedure, I hadn’t fully appreciated how many judgments about who “belongs” in graduate school happen long before any evaluation of research potential or intellectual fit. Once I understood the implications of that policy, I advocated to have it amended, and a student I would never have otherwise met was later admitted and enrolled.
The real work of equity is not expanding opportunity within unchanged systems but interrogating the systems themselves—especially when those systems quietly reward conformity.
That experience crystallized something for me. The student’s presence highlighted how even well-intentioned programs can struggle to value ways of thinking they were never designed to account for. The student, meanwhile, navigated those gaps with a practicality that exposed where the system itself needed adjustment.
The same design logic operates across American institutions that confuse neutrality with fairness. Even institutions that are equity forward, including my own, must navigate a shifting and often constraining federal landscape, making progress real, but necessarily incomplete.
This kind of exclusion is not unique to admissions policies. Across higher education, international students routinely navigate US systems calibrated to financial, cultural, and administrative norms that quietly penalize difference. More than 1 million international students are enrolled in US colleges and universities, and an analysis from the Association of American Universities estimates that international students contribute nearly $44 billion to the US economy annually. Yet research consistently shows that international students experience higher levels of social isolation than their domestic peers.
From a public health perspective, these barriers are not incidental—they are risk factors that function as chronic stressors. Uncertainty around visas, financial precarity, cultural dislocation, and exclusionary policies shape mental health and academic persistence long before a student ever sets foot on campus. Research shows that rates of anxiety, depression, and suicidality among international students have risen sharply over the past decade, even as access to culturally responsive mental health services remains uneven.
In public health, we name these design failures plainly: policy choices—not personal deficits. Improving the experience of international students is less about individual support than about whether institutions are willing to change the conditions they create.
What struck me most, though, was not my student’s resilience in the face of these barriers, but what institutions gain when those barriers are confronted. They were adept at finding workarounds where institutions offered only walls—and unapologetic about pointing out the walls. That resourcefulness did not just help them navigate the system; it revealed where the system itself needed to change.
The real work of equity is not expanding opportunity within unchanged systems but interrogating the systems themselves—especially when those systems quietly reward conformity.
We often talk about immigrants as beneficiaries of American opportunity. But in higher education, healthcare, research and beyond, immigrants are also architects of institutional improvement. They expose inefficiencies, challenge inherited assumptions, and force clarity around what we actually mean by merit.
Immigrants make up a disproportionate share of the US healthcare workforce, including physicians, researchers, and direct-care providers—roles that are essential as the country grapples with workforce shortages and widening health inequities.
Opportunity is not a one-way transaction. Institutions that welcome immigrants while resisting the changes their presence demands are not neutral—they are extractive.
Some people change institutions not by asking for permission, but by refusing explanations that don’t make sense. The question isn’t whether immigrants benefit from coming to the United States—the evidence is clear. The more uncomfortable and more important question is whether institutions are willing to reckon with how much they benefit from immigrants, and whether they are prepared to change to welcome them.