At two hospitals tucked in the quiet corners of Bellingham, Washington, an unfolding labor struggle cuts to the heart of the crisis in American healthcare. At PeaceHealth St. Joseph and PeaceHealth United General, hospitalists, including physicians and advanced practice providers, have walked off the job. However, this isn't a fight over salaries. It is a strike for the soul of their profession.
As members of the Union of American Physicians and Dentists (UAPD), these clinicians are demanding the right to advocate for their patients without fear of retaliation. They're calling out a system in which metrics and margins take precedence over urgent care and human dignity, discharges are prioritized over medical necessity and unsafe staffing has become the norm.
Despite a ruling from the National Labor Relations Board affirming their union, PeaceHealth, a large nonprofit hospital system, refuses to negotiate. The hospitalists are caught between two employers: Sound Physicians, which hires and pays them, and PeaceHealth, which controls their working conditions. Both point fingers, while the providers bear the burden.
We are striking to have a voice in our working conditions to ensure we can provide the best care for our patients.
In the following interviews, I speak with Katie Pernick (KP), Advanced Registered Nurse Practitioner (ARNP); Dr. Andy Radvany (AR), Hospitalist; and Joe Crane (JC), organizing coordinator, UAPD. They discuss how their struggle is rooted both in the specific conditions of Bellingham, Washington, and reflective of broader national dynamics, connecting clinical workplaces to the growing labor movement, the accelerating corporatization of healthcare, and a rising wave of collective action among white-collar and caregiving professions.
Can you describe specific examples of how PeaceHealth's policies have impacted patient care or safety in Bellingham or Sedro-Woolley?
 Katie Pernick stands outside PeaceHealth St. Joseph. (Photo: Brian Pernick)
Katie Pernick stands outside PeaceHealth St. Joseph. (Photo: Brian Pernick)
KP: For too long, healthcare has been dictated by insurance companies and hospital corporations. Healthcare decisions need to be made by physicians and advanced practice clinicians (APC), not by administration looking at what a patient is costing them. We are striking to have a voice in our working conditions to ensure we can provide the best care for our patients. For example, two years ago our contract was adjusted, without our input, to require us to see more patients. As hospitalists we are interacting with everyone: the patient, families, nurses, therapists, social workers, and specialists. That does not include the patients' imaging, lab work, and exam findings. All this information has to be integrated to provide a detailed plan of care. To do it for 16 or more acutely ill patients a day is a lot to ask. The increase in patient load has put patient care at risk and doesn't allow us the time needed to properly assess patients and their understanding of their illness, their symptoms, and conversation to allow the patient to have a voice in their care.
Another example is the early discharge requirement. Administration would like us to send patients home by 10:00 am. If I were to try to meet this requirement daily, I would have to cut down on time spent educating the patient on medications, their illness, and what to expect on return home. This doesn't consider that I would be seeing my sickest patients later in the day in favor of seeing my patients that are well enough to go home first. Hospital administration regularly adds busy work not related to patient care. This is more distraction from providing care for my patients.
No one's death should be part of an investment strategy.
Finally, over the years there have been several times where someone in administration has called me to tell me a patient had been in the hospital long enough and I needed to discharge the patient. In these situations, the administrator had not personally been to see the patient or assessed the patient, it was solely on how they looked in the chart and that according to insurance the patient should have been well by that time.
How has the refusal of PeaceHealth to recognize your union affected your ability to advocate for patients or voice safety concerns on the job?
KP: Patients trust us to care for them, and it is time for physicians and APCs to stand up and advocate on a larger scale for them. We want a say in our working conditions so we can provide the best care for patients and continue to do so. We want to address issues like the ones outlined above. I work with amazing people who truly care about their patients. When you are constantly asked to compromise your personal and moral ethics to care for patients it leads to moral injury, distress, and burn out. I can feel it happening to me on days when I have too many patients and feel like someone isn't getting my best.
Do you see your strike as part of a larger trend of healthcare worker organizing across the U.S.? If so, how?
KP: I hope so. Healthcare dictated by the moneymaking corporations isn't the best healthcare. I know so many physicians and APCs who are tired of not being able to provide appropriate care. We need to fight on a larger scale and stand together. American healthcare cannot continue in this way. Just this week the Hospitalists at Skagit Regional, another Sound Physicians site, voted in favor of unionizing by an overwhelming majority. I know several of my colleagues have been getting many questions about our experience from other hospitalists around the country.
Many countries with strong public health systems (like the U.K. or Canada) have unionized physicians. Do you see international models as informing your approach here?
 Joe Crane (in sunglasses) stands with striking workers. (Photo: Pierre King)
Joe Crane (in sunglasses) stands with striking workers. (Photo: Pierre King)
JC: The biggest problem with comparing the different systems isn't the public model versus nonprofit groups like PeaceHealth. The problem is that in America, we have companies like Sound Physicians that invest private equity money to make money from people in the worst moments of their lives. No one's death should be part of an investment strategy. Before we can start looking at how other unions in other countries are organized and fight back, we must fix a system that makes billions for investors when patients are sick and dying.
What role do corporate healthcare contractors like Sound Physicians play in undermining worker power and continuity of care?
KP: Estimates put 20% of healthcare dollars being spent on administrative tasks. Instead of turning down a patient for a life changing medication or medical device, what if we just said yes, they need this? Healthcare contractors like Sound add a layer of wasted medical dollars. I have two employers to answer to. More people sitting behind desks instead of directly caring for patients.
How has the community responded to the strike so far, and what do you want patients and families in this region to understand about your goals?
KP: I believe the majority of our community supports our union. PeaceHealth is a major local employer, and its decisions directly affect a wide segment of the population. Over the past year, its insurance policies have drawn criticism, and across the system, both in hospitals and clinics, providers are exhausted and overwhelmed. Our patients see it too; they can read the fatigue and strain on our faces.
Sound Physicians hospitalists have unionized under UAPD. PeaceHealth's advanced practice clinicians have done the same. Our nurses are in the midst of contract negotiations with Washington State Nurses Association, and our support staff have unionized with Service Employees International Union and are striking this week. When such a significant portion of an employer's workforce is organizing and protesting, it speaks volumes. PeaceHealth administrators often claim they are listening and seeking compromise, but if that were truly the case, how could so many workers be this frustrated?
It echoes the banking crisis of 2008, when profit-driven incentives corrupted the mortgage industry. Now, similarly perverse incentives are spreading through medicine like a cancer.
To our community, I want to say: We care deeply. We want the best for our patients. We want to return to work next week. But we also want a meaningful voice in the decisions that shape our ability to provide safe, ethical care. That means a seat at the table with PeaceHealth leadership.
To our colleagues, from dietary aides and housekeeping to radiology techs, phlebotomists, nurses, and beyond, we stand with you. We see the sacrifices you're making. That workers already struggling to make ends meet are willing to forgo a week's wages speaks to just how unfair these contracts are. Your courage underscores why this fight matters, for all of us.
How do you respond to the argument that physician unionization is incompatible with traditional notions of medical professionalism?
KP: When healthcare took a turn toward factory assembly line care and not an individual who needed tailored care, we went away from traditional medicine. When doctors are told they can only spend 20 minutes with a patient we turned away from traditional medicine. When I was told the reason I take so long to see patients is because I take too much time getting to know them, we turned away from traditional medicine.
Unionization is a return to the medical profession ideals in a time when corporations want to keep us quiet and subservient. The role of the Physician and APC's is to advocate for patients. Corporate healthcare took our professional autonomy; we want it back. They have not listened to us before. Unionization is the path back to traditional notions of medical professionalism. This is the path forward.
What do you think the growing labor unrest across industries, from Starbucks to Amazon to hospitals, says about the state of democracy and worker power in America?
JC: Something is broken in this country. More Physicians have unionized in the last two years than in the prior 20 years. As a union organizer, people might assume that this surge of unionization makes me happy; it does in the sense of seeing people come together and fight back, but it also breaks my heart how broken this system in our country is. Over $400 million per year are spent trying to crush workers who'd like to have a voice. Here in Bellingham, Washington, clinicians are taking to the strike line not for more money, but for the simple ask of wanting to care for their patients in the best possible way. Sound and PeaceHealth are taking money they made off sick human beings and are spending that money to try to make sure the physicians can't advocate for their patients. Our system is broken, but our UAPD members are standing up and fighting back, and we will win this fight.
 Dr. Andy Radvany protests outside the hospital. (Photo: Pierre King)
Dr. Andy Radvany protests outside the hospital. (Photo: Pierre King)
AR: Americans are pushing back against an economy where CEOs earn hundreds or even thousands of times more than their lowest-paid workers—a level of inequality rare in other developed nations. Executive pay has long outpaced reason, symbolizing a broken system.
Employee-owned WinCo offers a compelling alternative. It has created many millionaires among workers, without minting a single billionaire, proving that shared ownership can build wealth more equitably.
With a national election coming up, what would you like to see from political leaders in terms of healthcare reform and labor protections for clinicians?
JC: With the coming election, we need political leaders to stand up and fight with healthcare workers. We need to strengthen our labor laws. Your doctor shouldn't fear retaliation for advocating for their patients, and companies shouldn't profit from their constituents' sickness in a hospital. Doctors shouldn't have to strike just to be able to advocate for their patients. The politicians need to stand up and join the fight. If for no other reason, then they, too, will be patient someday. Do they want to be a profit margin on a spreadsheet or a human being getting the best possible help from a clinician who isn't afraid to speak up for their patient?
AR: I would like to see bills pushing back against C-Suite compensation, and private equity buyouts of healthcare interests. Medicine should not be for-profit business. The problem has grown exponentially, and hospital closures and lack of access are the result.
These are my patients, and their healthcare decisions should be made by me, not hospital administration.
Twenty years ago, many treatments and procedures that could be expedited to save money and keep patients out of the hospital are now delayed, until hospitalization becomes the only way to get them done quickly. This benefits hospital profits, not patients.
Meanwhile, corporate incentives have infiltrated even nonprofit health systems, distorting priorities. Executives chase bonus structures that reward volume and revenue, not outcomes or care. It's a systemic issue, deeper than any one boardroom. In many cases, leaders are doing exactly what they've been incentivized to do. It echoes the banking crisis of 2008, when profit-driven incentives corrupted the mortgage industry. Now, similarly perverse incentives are spreading through medicine like a cancer.
 The words, "Patients over profits" are projected onto the building of PeaceHealth St. Joseph. (Photo: Bellingham Trouble Makers)
The words, "Patients over profits" are projected onto the building of PeaceHealth St. Joseph. (Photo: Bellingham Trouble Makers)
If this strike succeeds, or fails, what precedent do you believe it will set for other hospitalists and healthcare workers nationwide?
KP: This strike is personal for me. This is my community. My patients are friends, friends of friends, parents of people I see at the gym, and the cashier that knows me from my weekly shopping. These are my patients, I don't know just the information in the chart (ie; imaging reports, lab work, vital signs). I know who has a sick cat at home, who is hoping to get out of the hospital before their grandchild's birthday next week, and who is scared to go home. These are my patients, and their healthcare decisions should be made by me, not hospital administration.
I hope our strike stirs more resistance from healthcare workers. We are the people that have the greatest opportunity to affect change in healthcare. It won't be able to come from the patients; they are effectively trapped by our healthcare system to accept what is given by their insurance. We need to stand for what is right, and we need to start now. Change is slow, but hope is already spreading.





 Katie Pernick stands outside PeaceHealth St. Joseph. (Photo: Brian Pernick)
Katie Pernick stands outside PeaceHealth St. Joseph. (Photo: Brian Pernick)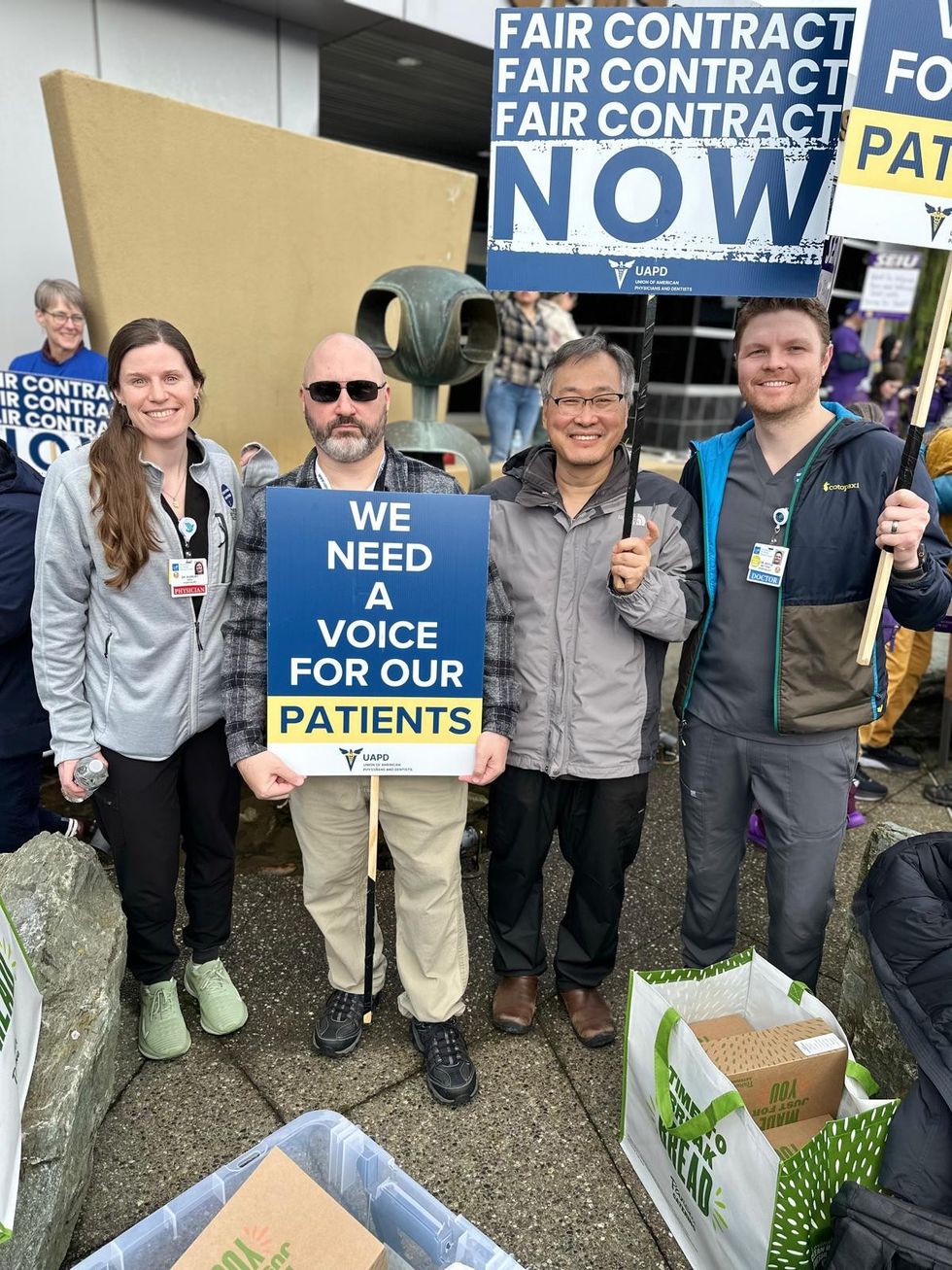 Joe Crane (in sunglasses) stands with striking workers. (Photo: Pierre King)
Joe Crane (in sunglasses) stands with striking workers. (Photo: Pierre King)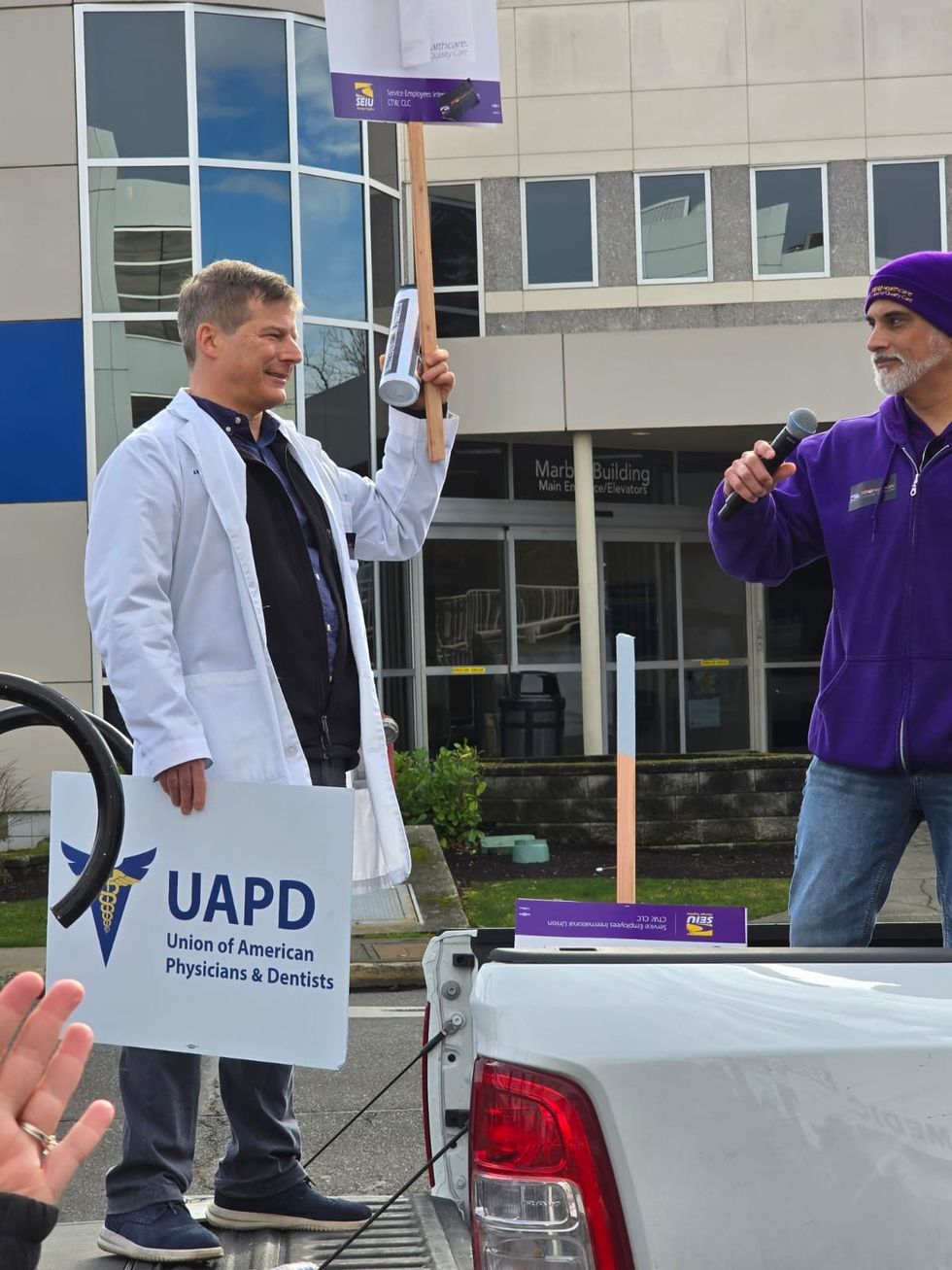 Dr. Andy Radvany
Dr. Andy Radvany  The words, "Patients over profits" are projected onto the building of PeaceHealth St. Joseph. (Photo: Bellingham Trouble Makers)
The words, "Patients over profits" are projected onto the building of PeaceHealth St. Joseph. (Photo: Bellingham Trouble Makers)