

SUBSCRIBE TO OUR FREE NEWSLETTER
Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.
5
#000000
#FFFFFF
To donate by check, phone, or other method, see our More Ways to Give page.


Daily news & progressive opinion—funded by the people, not the corporations—delivered straight to your inbox.
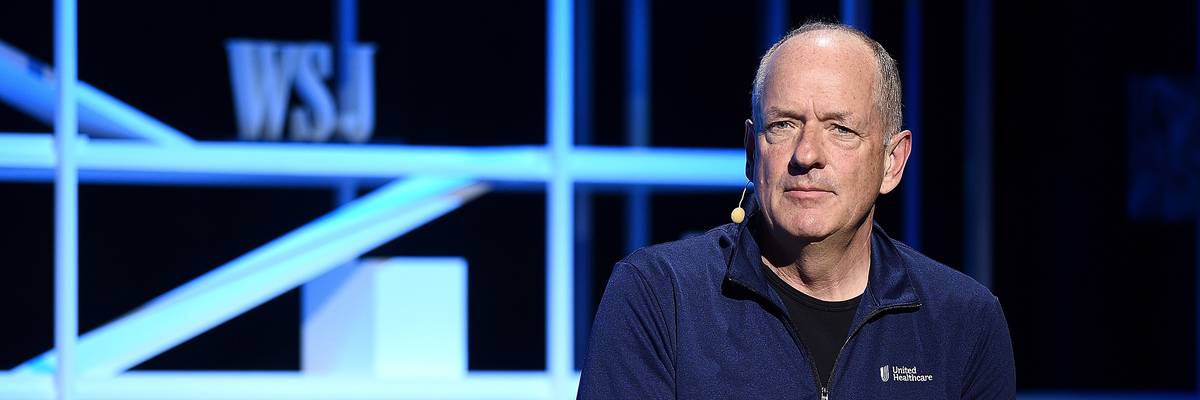
UnitedHealth Group CEO Andrew Witty attends an event on May 19, 2022 in New York City.
UnitedHealth CEO Andrew Witty told investors he "appreciates" the Biden administration's decision to slow the implementation of its Medicare Advantage reforms.
The chief executive of UnitedHealth Group told investors Friday that he "appreciates" the Biden administration's decision to more slowly implement its crackdown on overbilling in Medicare Advantage, a privately run, government-funded program that the Minnesota-based insurance behemoth touted as a key profit driver in its newly released first quarter earnings report.
UnitedHealth, one of the largest Medicare Advantage providers in the U.S., reported $91.9 billion in revenue for the first three months of 2023—15% growth year-over-year—and more than $8 billion in earnings from operations, exceeding analysts' expectations.
UnitedHealthcare, UnitedHealth Group's insurance business, "is pacing strongly to its outlook for another year of market-leading growth in serving more people through its Medicare Advantage offerings," the company said in its earnings release. The company said Friday that it added 655,000 new Medicare Advantage members in the first quarter of the year.
UnitedHealth's earnings report came after the company helped lead an aggressive lobbying campaign against new Biden administration rules aimed at limiting Medicare Advantage insurers' ability to overcharge the federal government by making patients appear sicker than they actually are.
According to The New York Times, UnitedHealth CEO Andrew Witty appeared on Capitol Hill in person to lobby against the proposed changes, which the lucrative Medicare Advantage industry falsely characterized as cuts to the program that now provides insurance to nearly half of the overall Medicare population.
Late last month, the Centers for Medicare and Medicaid Services (CMS) offered a number of concessions to the industry, agreeing to impose its policy changes over a period of three years instead of all at once and boosting Medicare Advantage payment rates by more than expected.
As STAT reported last week, Wall Street investors were "overjoyed" by the Biden administration's move, which drew criticism from progressive lawmakers and healthcare analysts who warned the slow phase-in will allow Medicare Advantage plans to continue their abusive practices. UnitedHealth, like other Medicare Advantage insurers, has been accused of wrongfully denying or attempting to deny patients necessary care, in some cases utilizing artificial intelligence to determine when to end coverage.
When it comes to excess billing, CMS recently estimated that overpayments to Medicare Advantage totaled $11.4 billion in fiscal year 2022—a significant drain on the Medicare trust fund.
Citing one industry analyst, STAT noted that UnitedHealth could reap $900 million in additional profit next year alone thanks to the administration's decision to delay full implementation of the reforms.
In an analysis published in February, former insurance executive Wendell Potter noted that UnitedHealth is one of just seven large for-profit insurance companies that now control 70% of the Medicare Advantage market, which is dependent on taxpayer money.
According to Potter, who now heads the Center for Health and Democracy, insurance giants UnitedHealth, Cigna, CVS/Aetna, Elevance, Humana, Centene, and Molina saw their combined revenues from taxpayer-supported programs grow 500% between 2012 and 2022.
"They've essentially been bailed out by taxpayers," Potter said of for-profit insurance giants like UnitedHealth in a recent interview with The American Prospect. "And members of Congress, and various administrations, have been just standing on the sidelines, not paying attention to what's been going on."
Dear Common Dreams reader, The U.S. is on a fast track to authoritarianism like nothing I've ever seen. Meanwhile, corporate news outlets are utterly capitulating to Trump, twisting their coverage to avoid drawing his ire while lining up to stuff cash in his pockets. That's why I believe that Common Dreams is doing the best and most consequential reporting that we've ever done. Our small but mighty team is a progressive reporting powerhouse, covering the news every day that the corporate media never will. Our mission has always been simple: To inform. To inspire. And to ignite change for the common good. Now here's the key piece that I want all our readers to understand: None of this would be possible without your financial support. That's not just some fundraising cliche. It's the absolute and literal truth. We don't accept corporate advertising and never will. We don't have a paywall because we don't think people should be blocked from critical news based on their ability to pay. Everything we do is funded by the donations of readers like you. Will you donate now to help power the nonprofit, independent reporting of Common Dreams? Thank you for being a vital member of our community. Together, we can keep independent journalism alive when it’s needed most. - Craig Brown, Co-founder |
The chief executive of UnitedHealth Group told investors Friday that he "appreciates" the Biden administration's decision to more slowly implement its crackdown on overbilling in Medicare Advantage, a privately run, government-funded program that the Minnesota-based insurance behemoth touted as a key profit driver in its newly released first quarter earnings report.
UnitedHealth, one of the largest Medicare Advantage providers in the U.S., reported $91.9 billion in revenue for the first three months of 2023—15% growth year-over-year—and more than $8 billion in earnings from operations, exceeding analysts' expectations.
UnitedHealthcare, UnitedHealth Group's insurance business, "is pacing strongly to its outlook for another year of market-leading growth in serving more people through its Medicare Advantage offerings," the company said in its earnings release. The company said Friday that it added 655,000 new Medicare Advantage members in the first quarter of the year.
UnitedHealth's earnings report came after the company helped lead an aggressive lobbying campaign against new Biden administration rules aimed at limiting Medicare Advantage insurers' ability to overcharge the federal government by making patients appear sicker than they actually are.
According to The New York Times, UnitedHealth CEO Andrew Witty appeared on Capitol Hill in person to lobby against the proposed changes, which the lucrative Medicare Advantage industry falsely characterized as cuts to the program that now provides insurance to nearly half of the overall Medicare population.
Late last month, the Centers for Medicare and Medicaid Services (CMS) offered a number of concessions to the industry, agreeing to impose its policy changes over a period of three years instead of all at once and boosting Medicare Advantage payment rates by more than expected.
As STAT reported last week, Wall Street investors were "overjoyed" by the Biden administration's move, which drew criticism from progressive lawmakers and healthcare analysts who warned the slow phase-in will allow Medicare Advantage plans to continue their abusive practices. UnitedHealth, like other Medicare Advantage insurers, has been accused of wrongfully denying or attempting to deny patients necessary care, in some cases utilizing artificial intelligence to determine when to end coverage.
When it comes to excess billing, CMS recently estimated that overpayments to Medicare Advantage totaled $11.4 billion in fiscal year 2022—a significant drain on the Medicare trust fund.
Citing one industry analyst, STAT noted that UnitedHealth could reap $900 million in additional profit next year alone thanks to the administration's decision to delay full implementation of the reforms.
In an analysis published in February, former insurance executive Wendell Potter noted that UnitedHealth is one of just seven large for-profit insurance companies that now control 70% of the Medicare Advantage market, which is dependent on taxpayer money.
According to Potter, who now heads the Center for Health and Democracy, insurance giants UnitedHealth, Cigna, CVS/Aetna, Elevance, Humana, Centene, and Molina saw their combined revenues from taxpayer-supported programs grow 500% between 2012 and 2022.
"They've essentially been bailed out by taxpayers," Potter said of for-profit insurance giants like UnitedHealth in a recent interview with The American Prospect. "And members of Congress, and various administrations, have been just standing on the sidelines, not paying attention to what's been going on."
The chief executive of UnitedHealth Group told investors Friday that he "appreciates" the Biden administration's decision to more slowly implement its crackdown on overbilling in Medicare Advantage, a privately run, government-funded program that the Minnesota-based insurance behemoth touted as a key profit driver in its newly released first quarter earnings report.
UnitedHealth, one of the largest Medicare Advantage providers in the U.S., reported $91.9 billion in revenue for the first three months of 2023—15% growth year-over-year—and more than $8 billion in earnings from operations, exceeding analysts' expectations.
UnitedHealthcare, UnitedHealth Group's insurance business, "is pacing strongly to its outlook for another year of market-leading growth in serving more people through its Medicare Advantage offerings," the company said in its earnings release. The company said Friday that it added 655,000 new Medicare Advantage members in the first quarter of the year.
UnitedHealth's earnings report came after the company helped lead an aggressive lobbying campaign against new Biden administration rules aimed at limiting Medicare Advantage insurers' ability to overcharge the federal government by making patients appear sicker than they actually are.
According to The New York Times, UnitedHealth CEO Andrew Witty appeared on Capitol Hill in person to lobby against the proposed changes, which the lucrative Medicare Advantage industry falsely characterized as cuts to the program that now provides insurance to nearly half of the overall Medicare population.
Late last month, the Centers for Medicare and Medicaid Services (CMS) offered a number of concessions to the industry, agreeing to impose its policy changes over a period of three years instead of all at once and boosting Medicare Advantage payment rates by more than expected.
As STAT reported last week, Wall Street investors were "overjoyed" by the Biden administration's move, which drew criticism from progressive lawmakers and healthcare analysts who warned the slow phase-in will allow Medicare Advantage plans to continue their abusive practices. UnitedHealth, like other Medicare Advantage insurers, has been accused of wrongfully denying or attempting to deny patients necessary care, in some cases utilizing artificial intelligence to determine when to end coverage.
When it comes to excess billing, CMS recently estimated that overpayments to Medicare Advantage totaled $11.4 billion in fiscal year 2022—a significant drain on the Medicare trust fund.
Citing one industry analyst, STAT noted that UnitedHealth could reap $900 million in additional profit next year alone thanks to the administration's decision to delay full implementation of the reforms.
In an analysis published in February, former insurance executive Wendell Potter noted that UnitedHealth is one of just seven large for-profit insurance companies that now control 70% of the Medicare Advantage market, which is dependent on taxpayer money.
According to Potter, who now heads the Center for Health and Democracy, insurance giants UnitedHealth, Cigna, CVS/Aetna, Elevance, Humana, Centene, and Molina saw their combined revenues from taxpayer-supported programs grow 500% between 2012 and 2022.
"They've essentially been bailed out by taxpayers," Potter said of for-profit insurance giants like UnitedHealth in a recent interview with The American Prospect. "And members of Congress, and various administrations, have been just standing on the sidelines, not paying attention to what's been going on."