August, 26 2009, 08:50am EDT

For Immediate Release
Contact:
Shum Preston, 510-273-2276 or Liz Jacobs, 510-273-2232
Many Hospitals Are Not Ready for H1N1: Nurse Survey Shows Deficiencies in Hospital Swine Flu Readiness
Data from 190 Healthcare Facilities in Nine States from California to Maine
NATIONWIDE
A patient health and safety survey of 190 American hospitals
from coast to coast compiled by registered nurses in eight
different states finds that a disturbing number of our nation's
healthcare facilities are not prepared for the coming H1N1/swine
flu pandemic, according to results released today by the
California Nurses Association/National Nurses Organizing
Committee.
The data reflects a survey conducted over the past four weeks
by RNs in hospitals in Arizona, California, Florida, Illinois,
Maine, Minnesota, Nevada, Pennsylvania, and Texas. And it
comes just a day after release of a report from the President's
Council of Advisors on Science and Technology predicting nearly
2 million Americans could be hospitalized due to swine flu
infections this winter, and as many as 90,000 could die, nearly
triple the deaths that occur in a normal flu season.
What the RNs reported are wide gaps in safety gear, infection
control training, and post-exposure procedures. Among key
findings:
- At more than one-fourth of the hospitals, nurses
cite inadequate isolation of swine flu patients, increasing the
risk of infection to others. - Nurses at 15 percent of hospitals do not have access
to the proper respirator masks, exposing nurses and patients to
infection; at up to 40 percent of the hospitals,
nurses are expected to re-use masks, in violation of
Centers for Disease Control
Guidelines. - At 18 percent of the hospitals, RNs report that
nurses have become infected; one Sacramento, Calif. RN has
already died.
CNA/NNOC is calling on all hospitals to adhere to the highest
standard of protection for patients and nurses to combat the
expected onslaught of new cases this fall and winter, and urging
legislators to strengthen public protections.
"These continuing problems increase the risk that many
hospitals will become vectors for infection, with inadequate
patient protections leading to a spread of the pandemic among
other patients, their friends, family, and caregivers, and the
surrounding community," warned Deborah Burger, RN, CNA/NNOC
co-president. "What we're hearing from around the country is
dangerous to patient health and safety, but with smart and
clinically appropriate leadership we can fix policies in time
for the upcoming pandemic."
On Wednesday, nurses at more than 50 of these
hospitals, mostly large hospital systems, will hold actions to
demand hospital administrators immediately implement safety
improvements for nurses and patients. Contact CNA/NNOC to
find out about what nurses are doing in your area.
CNA/NNOC leaders will also be testifying in a joint
California Senate hearing in Sacramento Thursday on preparedness
for swine flu in the state's health and education systems.
The hearing is at 9 a.m. in Room 112 at the State
Capitol.
"This report should serve as a wake-up to hospital
management, policy makers, and healthcare workers across the
country. We need to urgently increase our readiness,"
Burger said. "We do not yet have a complete picture of the
morbidity of the H1N1 pandemic. But that is no justification for
hospitals making inadequate preparations and endangering the
health and safety of patients and their community. When
September comes, we expect that infection rates of H1N1 will
spike due to the beginning of the school year, prompting
overcrowded emergency rooms, which will put our public health
readiness to the test."
"The swine flu is not the type of flu we are used to.
This pandemic will stress every aspect of our healthcare
system. Hospitals must be proactive in protecting the
public," said Houston RN Terry Hardin.
"The state of Maine has identified over 300 cases of H1N1
infection, resulting in at least 19 hospitalizations and one
death," said Cokie Giles, EMMC, president of Maine State Nurses
Association/NNOC. "A recent survey of our membership
indicates that there may be some areas of serious concern
regarding preparedness policies. We are calling on
MSNA/NNOC represented facilities to ensure that patients and
nurses are protected to the fullest extent from exposure to
H1N1."
"It is important for hospitals to meet full safety standards
for swine flu so that our patients and our nurses are
protected," said Temple University Hospital RN Patricia Eakin,
president of the Pennsylvania Association of Staff Nurses and
Allied Professionals/NNOC.
"I don't know how the local hospitals will staff up for the
pandemic. Nurses at my institution don't accrue sick time, we
use our accrued vacation time to call out sick. We also
work short [staffed] instead of having a replacement when
someone does call out. In these economic times, you tell
me who will be staffing the hospitals?" said Tampa Bay area RN
Peggy Bowen.
Illinois hospitals, says Chicago RN Brenda Langford, "are not
prepared to deal with this pandemic. We have provided our
copies of our surveys to management and they have not moved to
change our practice to be in compliance with the recommendation
set for by the CDC. If the Cook County Health and Hospital
System won't make these needed changes and the Cook County
Department of Public Health won't support our efforts to protect
the nurses and the public, it is left up to the NNOC to make
sure these needed protections are implemented."
Findings of the survey include:
- Half the hospitals have seen infected patients. At 18
percent, RNs have been infected, nurses say. - Nurses at 15 percent of hospitals report that they do not
have access or only some have access to the appropriate N95
respirator masks, and at 19 percent of the hospitals all or some
masks were not "fitted," to ensure their effectiveness against
the virus - More than one in five, 22 percent of the facilities, do not
have enough masks, say nurses. - At almost 40 percent of those which do have sufficient
masks, all or some of the masks are expected to be reused, say
nurses. That puts nurses and patients at risk of infection and
violates CDC guidelines which say all healthcare personnel who
enter rooms of patients in isolation for H1N1 should wear a
fit-tested disposable N95 mask, and that the masks should not be
reused. - Nurses at 26 percent of hospitals report that infected
patients are not being properly isolated, in appropriately
ventilated rooms, raising the possibility of the infection
spreading to others in the facility. At nearly a third of the
facilities, proper infection controls are not being
followed. - Nurses at fewer than half of facilities (49 percent) report
that they have been adequately trained on H1N1 issues, including
identification of infected patients, and procedures for caring
for these patients. - Nurses at only 35 percent of facilities report that they are
guaranteed adequate sick leave if they become ill while caring
for a patient, penalizing them for appropriately staying home
while infectious.
These numbers are borne out by the controversies that have
been reported at hospitals across the country. Examples
include:
- At the University of California Davis Medical Center (near
Sacramento), a patient who subsequently died from H1N1 was
transferred to an intensive care unit as the patient's condition
deteriorated. But rather than be kept in strict isolation with
proper ventilation, the door to the patient's room was kept open
the entire time, placing other high-risk patients, visitors, and
caregivers at risk. - Nurses at Temple University Hospital, a major acute-care
hospital in Philadelphia, are concerned that the level of
preparedness is not sufficient. The hospital has yet to make
clear to nurses its plans and procedures for dealing with H1N1
which is expected to worsen with the start of the school year.
The nurses are already seeing an influx of more patients due to
the closure of one of Temple's nearby facilities, Northeastern
Hospital, and are concerned that without better preparation and
sufficient staff, the anticipated influx of patients due to the
pandemic would be especially dangerous. - At Sutter Solano Medical Center in Vallejo, Calif., there
were not enough masks to deal with three infected patients in
the ICU. Within short order, approximately 10 nurses were
affected. The state office of occupational health and
safety is investigating. - Nurses report that a Kaiser Hospital South Sacramento has
informed patients and visitors that N95 respirator masks are not
necessary and that simple "surgical" masks will suffice, which
directly contravenes standards issued by every government
agency. - Nurses at Los Alamitos Medical Center near Los Angeles
report that Tenet has eliminated sick benefits that would ensure
nurses could afford to take time away from work if they develop
symptoms.
In conjunction with the report, CNA/NNOC is releasing a list
of demands - "The Nurses' Swine Flu Safety
Agenda" - to adequately prepare for this
pandemic.
- Minimize infection of hospital patients and workers by
strict adherence to the highest standard of infection control
procedures, including identification and isolation with
appropriate ventilation of infected patients - All hospital workers and visitors must be provided with
appropriate protection gear at the highest government standards,
including N95 respirator masks or better for all who enter the
isolation room of a confirmed or suspected H1N1 patient. - Guarantee all patients and workers full transparency after
any exposures to H1N1, in as timely a manner as possible - Healthcare workers and facility visitors must receive full
information and guidelines on risk exposure and facility
infection control recommendations - Any RN who is unable to work due to contracting a
communicable or infectious disease identified or treated in his
or her hospital/clinic shall be guaranteed sick leave, not face
disciplinary action, and shall be presumptively eligible for
workers' compensation benefits - Implement a moratorium on any closures of emergency rooms,
layoffs of direct healthcare personnel, and reductions of
hospital beds. - Federal guidelines for protection must be developed that are
consistent across agencies - Disposable respirator masks must not be re-used. In the
event of a demonstrated national mask shortage, facilities
should adhere to government recommendations on mask
conservation.
National Nurses United, with close to 185,000 members in every state, is the largest union and professional association of registered nurses in US history.
(240) 235-2000LATEST NEWS
'Damning' Independent Probe Finds Israel Has Yet to Provide Evidence Against UNRWA
The U.S. House on Saturday passed a bill including a prohibition on funding the agency, due to Israel's unsubstantiated claims that UNRWA employees have terrorism links.
Apr 22, 2024
Countries that have continued to suspend their funding of the United Nations' top relief agency in the occupied Palestinian territories were left with "no room" to justify their decision, said critics on Monday as an independent investigation into Israel's allegations against the organization revealed Israeli officials have ignored requests to provide evidence to support their claims.
Catherine Colonna, the former foreign minister of France, released her findings in a probe regarding Israel's claims that a significant number of employees of the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA) were members of terrorist groups.
Nearly three months after U.N. Secretary-General António Guterres commissioned the report, Colonna said Israel "has yet to provide supporting evidence" of its allegation that "a significant number of UNRWA employees are members of terrorist organizations."
Colonna's findings were bolstered by an investigation led by the Raoul Wallenberg Institute of Human Rights and Humanitarian Law in Sweden, the Chr. Michelsen Institute in Norway, and the Danish Institute for Human Rights, which separately sought evidence from Israel.
"Israeli authorities have to date not provided any supporting evidence nor responded to letters from UNRWA in March, and again in April, requesting the names and supporting evidence that would enable UNRWA to open an investigation," said the Nordic groups.
The reports come nearly three months after Israel made its initial allegation that 12 UNRWA employees took part in the October 7 Hamas-led attack on southern Israel, a claim that prompted the United States—the largest international funder of the agency, which subsists mainly on donations—to swiftly halt its funding. Israel also claimed that as many as 12% of UNRWA's employees were members of terrorist organizations.
As Common Dreamsreported at the time, Israel's announcement came hours after the International Court of Justice (ICJ) issued a preliminary ruling that found Israel was "plausibly" committing a genocide in Gaza by relentlessly striking the enclave and blocking almost all humanitarian aid to its 2.3 million people.
The Biden administration has dismissed the ICJ's finding.
The United States' suspension of UNRWA funding set off a domino effect, leading at least 15 countries to freeze their contributions, even though the U.N. had reported a month earlier that Israel's air, land, and sea blockade on Gaza was pushing hundreds of thousands of civilians into starvation.
Countries including Sweden, Japan, France, and Australia have reinstated their funding of the agency in recent weeks, citing concerns about the intensifying humanitarian crisis in Gaza—where more than two dozen children have died of starvation so far—and Israel's lack of evidence.
Lawmakers in the U.S., which provides nearly $344 million to UNRWA annually, included a prohibition on funding for the agency in its foreign aid bill that passed in the House of Representatives on Saturday, while the United Kingdom has said it would make a decision about resuming funding after the Colonna report was released.
"The report leaves no room for Britain to justify the continued suspension of funds," said the independent news group Declassified U.K.
Colonna's report, which was accepted by Guterres Monday, noted that UNRWA is more rigorous than other U.N. agencies in its internal oversight of its staff and their neutrality.
"The review revealed that UNRWA has established a significant number of mechanisms and procedures to ensure compliance with the humanitarian principles, with emphasis on the principle of neutrality and that it possesses a more developed approach to neutrality than other similar U.N. or NGO entities," reads the report.
Guterres called on donor countries to "fully cooperate in the implementation of the recommendations" of the report.
"Moving forward, the secretary-general appeals to all stakeholders to actively support UNRWA, as it is a lifeline for Palestine refugees in the region," said the U.N. chief's office in a statement.
Despite the U.K.'s claim that it would review Colonna's report to determine whether to resume funding, The Guardianreported the government was "unlikely" to make a prompt decision based on the findings, as Conservative lawmakers have urged Foreign Secretary David Cameron against doing so.
The continued suspension of donations, said U.K.-based researcher and activist Gary Spedding, "is unjustifiable and at total odds with the rest of our allies (except the USA) who resumed funding."
"Our government has so much to answer for regarding the decision to pause funding without any evidence whatsoever, then sustain that decision even while other allies resumed and Palestinians in Gaza starved and died from sickness and disease, and even now we still haven't resumed," said Spedding. "We must have accountability and answers. Why did the government pause funding to begin with despite no evidence being presented by Israel? Why have we joined in on damaging UNRWA as part of Israel's plan to dismantle it? Why are Palestinian lives and rights worth so little?"
Colonna's report, said Quincy Institute for Responsible Statecraft executive vice president Trita Parsi, is "not only damning for Israel."
"It is also damning for all the Western countries," he said, "that cut funding for UNRWA on mere (now debunked) accusations by Israel."
Keep ReadingShow Less
Led by US, Global Military Spending Surged to Record $2.4 Trillion Last Year
"Can we get some healthcare please, or maybe feed some of the 40 million+ Americans who can't get enough food?" asked the watchdog group Public Citizen.
Apr 22, 2024
New research published Monday shows that global military spending increased in 2023 for the ninth consecutive year, surging to $2.4 trillion as Russia's assault on Ukraine and Israel's war on the Gaza Strip helped push war-related outlays to an all-time high.
The Stockholm International Peace Research Institute (SIPRI) recorded military spending increases in every geographical region it examined last year, from Europe to Oceania to the Middle East. Last year's global increase of 6.8% was the largest since 2009, SIPRI said.
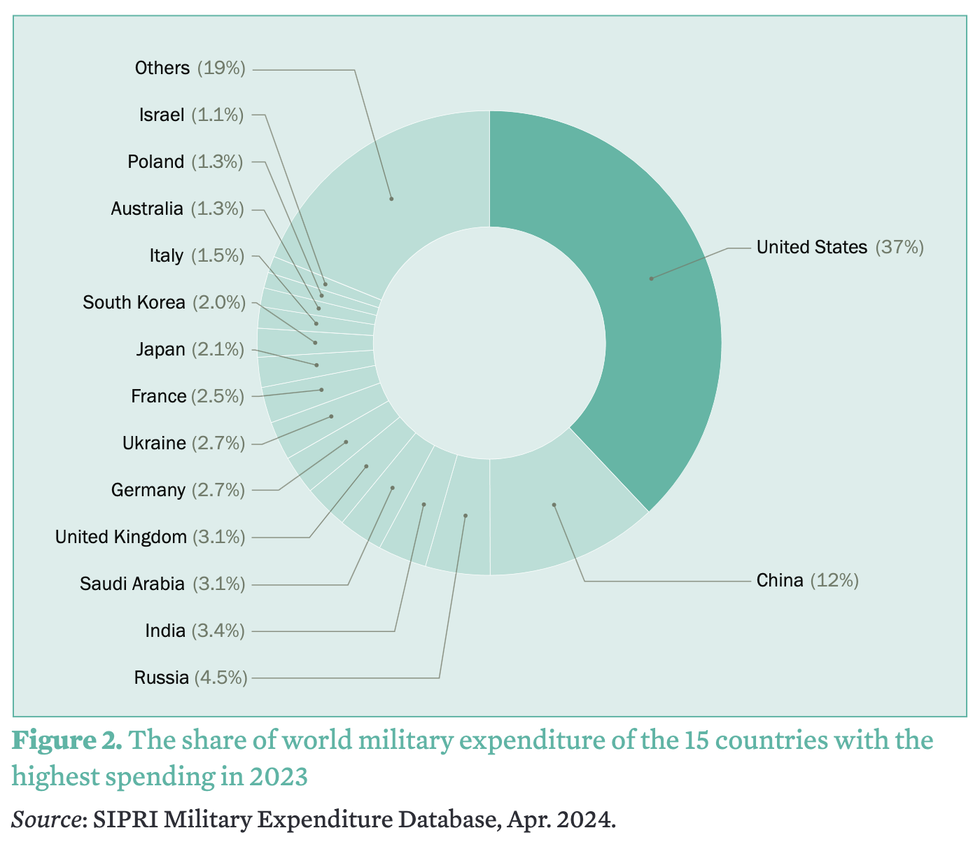
The United States was by far the largest military spender at $916 billion in 2023, up 2.3% compared to the previous year. The next biggest spender was China, which poured an estimated $296 billion into its military last year—three times less than the U.S.
"Can we get some healthcare please, or maybe feed some of the 40 million+ Americans who can't get enough food?" asked the watchdog group Public Citizen in response to SIPRI's report, which found that the U.S. accounted for 37% of the world's total military spending last year.
A separate analysis of U.S. military spending in 2023 found that 62% of the country's federal discretionary budget went to militarized programs, leaving less than half of the budget for healthcare, housing, nutrition assistance, education, and other domestic priorities.
Together, SIPRI found, the top five biggest military spenders last year—the U.S., China, Russia, India, and Saudi Arabia—accounted for 61% of global military outlays.
"The unprecedented rise in military spending is a direct response to the global deterioration in peace and security," Nan Tian, senior researcher with SIPRI's Military Expenditure and Arms Production Program, said in a statement. "States are prioritizing military strength but they risk an action-reaction spiral in the increasingly volatile geopolitical and security landscape."
In the Middle East, military spending jumped by 9% last year—the highest annual growth rate in the past decade. Israel, which relies heavily on weapons imports from the U.S., spent 24% more on its military last year than in 2022, according to SIPRI, an increase fueled by the country's devastating assault on Gaza.
SIPRI found that NATO's 31 member countries dumped a combined $1.3 trillion into military expenditures in 2023, accounting for 55% of the global total.
U.S. military spending, which is poised to continue surging in the coming years, made up 68% of NATO's 2023 total.
Keep ReadingShow Less
IDF Kills 18 Children in Rafah Hours After US House Approves Billions in Military Aid
"Members of Congress should understand that approving more military aid could subject them to personal liability for aiding and abetting an ongoing genocide in Gaza."
Apr 22, 2024
Hours after the U.S. House approved legislation that would send billions of dollars in additional military aid to Israel, the country's forces killed nearly two dozen people in Rafah, the southern Gaza city where more than half of the enclave's population is sheltering.
Gaza health officials said Sunday that the weekend strikes on Rafah—a former "safe zone" that Israel has been threatening to invade for weeks—killed 22 people, including 18 children. The Associated Pressreported that the first of the Israeli strikes "killed a man, his wife, and their 3-year-old child, according to the nearby Kuwaiti Hospital, which received the bodies."
"The woman was pregnant and the doctors saved the baby, the hospital said," AP added. "The second strike killed 17 children and two women from an extended family."
Israeli forces have killed more than 14,000 children in Gaza since October, but the Biden administration and American lawmakers have refused to back growing international calls to cut off the supply of weaponry and other military equipment even as U.S. voters express support for an arms embargo.
The measure the House approved on Saturday includes $26 billion in funding for Israel, much of which is military assistance.
"Just a day after the House voted to send $14 billion in unconditional military funding to [Israeli Prime Minister Benjamin] Netanyahu's campaign of death and destruction, he bombed the safe zone of Rafah AGAIN, killing 22 Palestinians, of which 18 were CHILDREN!" U.S. Rep. Delia Ramirez (D-Ill.), one of the 58 House lawmakers who voted against the legislation, wrote on social media late Sunday.
"History books will write about today and the past seven months, and how our nation's leaders lacked the courage and moral clarity to stand up to a tyrant," she added. "Shameful."
The military aid package for Israel now heads to the U.S. Senate, which is set to consider the bill early this week. U.S. President Joe Biden, who has continued to greenlight arms sales to Israel amid clear evidence of war crimes, is expected to sign the measure if it reaches his desk.
"Rather than sending more weapons to Israel, Congress should declare an immediate arms embargo on Israel."
U.S. law prohibits "arms transfers that risk facilitating or otherwise contributing to violations of human rights or international humanitarian law," according to a White House memo issued in February. The U.S. State Department has said repeatedly that it has not found Israel to be in violation of international law, a position that runs directly counter to the findings of leading humanitarian organizations and United Nations experts.
The investigative outlet ProPublicareported last week that a "special State Department panel recommended months ago that Secretary of State Antony Blinken disqualify multiple Israeli military and police units from receiving U.S. aid after reviewing allegations that they committed serious human rights abuses" prior to the October 7 Hamas-led attack on southern Israel.
"But Blinken has failed to act on the proposal in the face of growing international criticism of the Israeli military's conduct in Gaza, according to current and former State Department officials," ProPublica noted.
Sarah Leah Whitson, executive director of Democracy for the Arab World Now (DAWN), said in a statement Sunday that senators "should reject sending additional weapons to Israel not only because our laws prohibit military aid to abusive regimes, but because it's extremely damaging to our national interests."
DAWN's advocacy director, Raed Jarrar, added that "at a time when Israel is bracing for International Criminal Court arrest warrants against its leaders, members of Congress should understand that approving more military aid could subject them to personal liability for aiding and abetting an ongoing genocide in Gaza."
"Rather than sending more weapons to Israel," said Jarrar, "Congress should declare an immediate arms embargo on Israel."
Keep ReadingShow Less
Most Popular